While mild cognitive impairment frequently goes undiagnosed, millions of Americans are thought to suffer from the condition. MCI can be difficult to identify during a regular checkup at the doctor’s office, a visit that’s normally too short for a full cognitive evaluation.
Many people dealing with mild cognitive impairment may also be hesitant to tell their doctors about any symptoms they’re experiencing or might not even realize there’s a problem.
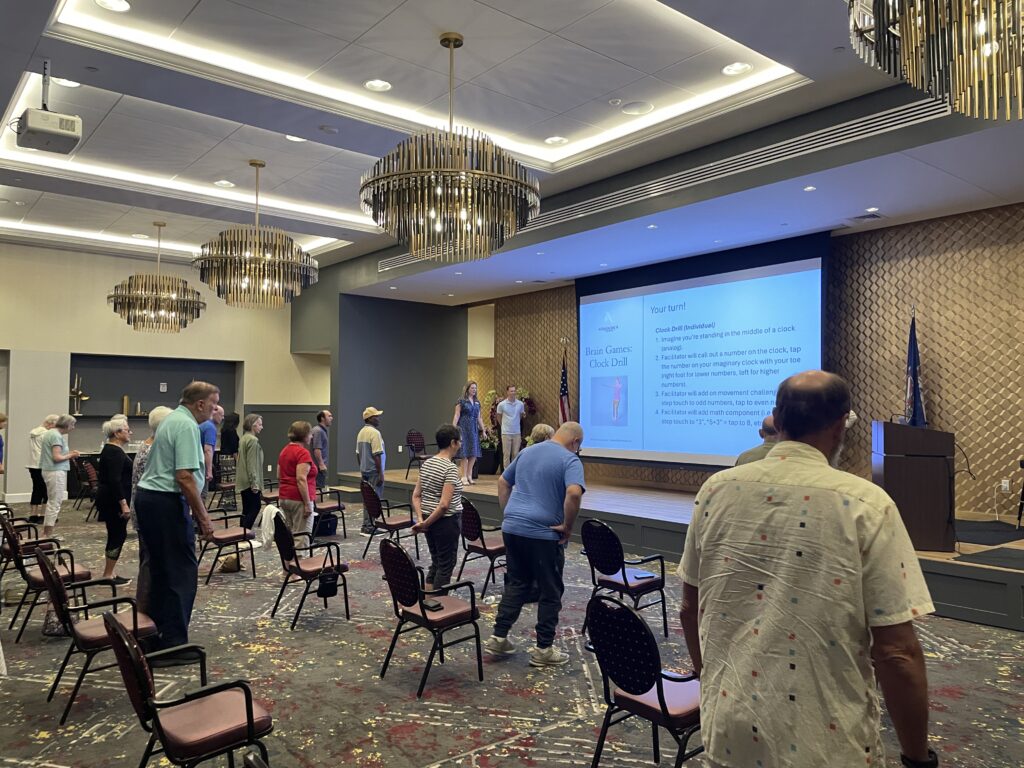
Harbor’s Edge is renowned for its Independent Living apartments, but the community has relaunched The Center for Memory Support to help those struggling with cognitive impairment issues. We can help you navigate this journey and support your loved ones both physically and mentally.
What is MCI?
MCI most often stems from a neurodegenerative disorder, such as Alzheimer’s disease, but cognitive impairments could also be caused by a reversible issue, like vitamin deficiency, lack of quality sleep, or medication change. If MCI is due to a neurodegenerative condition, it can progress to dementia, though the timeline of progression is widely varied. Roughly 10-15 percent of people with MCI are diagnosed with dementia each year.
Mild cognitive impairment occurs before dementia. MCI is where there are more thinking problems than expected at a certain age, but there’s still a level of independence being maintained for daily functioning. It can be difficult to know what’s normal forgetfulness that comes with age, and what’s a sign that something may be wrong. One indication of possible MCI is if a person has to start implementing strategies to help them keep up with basic activities, like leaving notes throughout the house for themselves so they remember the things they need to do throughout the day.
How is it diagnosed?
Screening for M.C.I. and dementia often takes place in primary care doctor’s offices. Medicare, which people are eligible for starting at 65, requires physicians to assess cognitive health at the annual wellness visit. However, these screens can be as basic
as asking the patient whether they’ve noticed any issues with their memory. Often, a physician only initiates a longer dementia test if the patient or a family member has expressed concern.
There are a couple common tests used to diagnose MCI and dementia. Both the Mini-Mental State Exam and the Montreal Cognitive Assessment take about ten minutes and consist of questions to evaluate memory, attention, verbal ability and general awareness. These tests use scoring thresholds to determine MCI or dementia, but they aren’t the end-all, be-all. Many doctors consider the patient’s and family members’ evaluations to be equally as – if not more – important.
If a person is diagnosed with MCI, they may be referred for more extensive cognitive testing with a neuropsychologist, where they will receive other assessments, like brain scans and blood tests, to determine what the underlying cause of their issue might be.
A diagnosis alone can’t explain what’s causing a person’s symptoms, which is the best way to determine how concerned a patient and their family should be and what next steps should be taken.
Our Center for Memory Support is a great next option to give you peace of mind that your loved one is being supported and cared for in an engaging community.
The first step is always a cognitive health evaluation. If you’re concerned about your loved one’s memory, encourage them to visit a doctor and explain your concerns. Start thinking about cognitive health evaluation as part of the physical exam. Just like our heart and lungs are evaluated, our brains should be too.